DREAMers Moms Tijuana – Yolanda Varona
In 2011, Yolanda Varona was unexpectedly separated from her children at the end of a trip across the border. She was deported to Mexico.
As Varona found ways to connect with her children and worked toward being with them again, she helped other deported mothers to find services and resources. Varona became the Founder and Director of DREAMers Moms in Tijuana, Mexico, as many of the women, Varona worked with were mothers of children with US citizenship or qualify for Deferred Action for Childhood Arrivals (DACA), otherwise known as DREAMers.
In 2019, Mari McMenamin, Dana Schuerholz and I traveled to San Diego, California and Tijuana, Mexico to cover border stories and listened to Varona’s story of deportation and efforts to connect with her daughter.
Producers: Mari McMenamin, Laura Florez. Special thanks to Magdaleno Rose-Avila of Building Bridges for inspiring us to pick up this story and for connecting us to the speakers.
Photos: Dana Schuerholz, Mari McMenamin
Families in Solidarity with Palestine
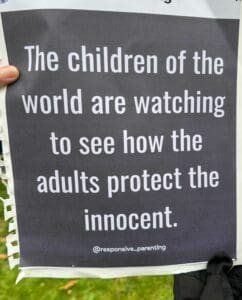
In Gaza, Israeli attacks have killed 8,000 women and children (70% of fatalities). Today, the two largest hospitals in Gaza have stopped functioning as they’ve run out of fuel and are surrounded by Israeli forces.
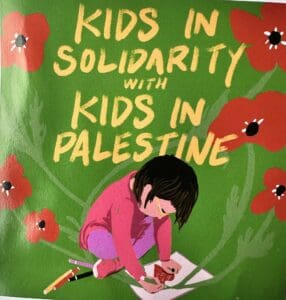
Meanwhile, yesterday, 300-400 hundred people gathered in Seattle’s Columbia Park for a Ceasefire march around the block and rally for families and children. Participants sang songs, painted murals and prayer flags for Palestine, and wrote postcards addressed to state elected officials to demand a ceasefire.
Listen to some sounds and voices from the event. You may hear the rain in some of the clips.
A longer highlight of this event will broadcast tomorrow on KBCS during the Grit at 7 am.
Producer: Yuko Kodama
Photos: Yuko Kodama
second row – Miwa Nietering (age 6), Nazia Siddiqi
third row – Rose Waterstone and Cypress Waterstone (age 10)
fourth row – Loren, Zachary, Theo, Tony and Didi; mural of handprints
sixth row – the march was around the block
seventh row – Macy Ratliffe “Don’t let the world forget about us. Free Palestine”
eighth row – table to write post cards to Washington state elected officials
ninth row – artwork by Ruth Wilson Gilmore
tenth row – art tent to contribute to the mural and to create prayer flags
Teaching Lushootseed to Toddlers
Lushootseed is the language spoken by Coast Salish tribes in the greater Seattle area and north to Skagit River Valley near Bellingham and Whidbey Island, and south to Olympia and Shelton. In 1819, Congress passed the Civilization Fund Act to assimilate indigenous youth to western culture. The policy authorized forcible separation of indigenous children from their families to be sent to boarding schools far away, where they were to be stripped of their language, culture and religious practices. It wasn’t until the 1970’s that this practice was outlawed. This caused a severe disruption in likelihood for traditional practices and lifestyles to continue.
Today, members of these communities are reawakening their native tongue through education to everyone from 6 month olds, elementary and high school students and adults.
Jasmyne Diaz is an enrolled Tulalip member and shares a peek into her work of teaching Lushootseed language as a Teacher Assistant to six-month to two-year old children in Tulalip, Washington through the Tulalip Lushootseed Language Program
Producers: Laura Florez and Yuko Kodama
Supporting Families Through the Pandemic
Gerald Donaldson is a Family Support Worker at Leschi Elementary School in the Seattle Public School System. He assists families who need help, so the children at Leschi can thrive in school.
Donaldson describes the challenges through the pandemic (from our interview with him last spring), and gives a more recent update of where many of his families are in their support needs now.
Kids, Schooling, Work and Home During Stay at Home Orders
As families hunker down at home and share time, electronic devices and space, here are some nuggets to chew on from school psychologist and Co Founder of Sproutable, Julietta Skoog.
Adverse Childhood Experiences and Long Term Health Impacts
A study on the impacts of adverse childhood experiences (ACE), including exposure to emotional, physical, sexual abuse, or household dysfunction on adult long term health was published in 1998. The study found a relationship of ACE exposure to increased heart disease, cancer and chronic lung disease in adulthood. Since this study, many public health agencies have had an eye on this issue as they strategize for better health outcomes in our communities.
Dr. Benjamin Danielson is a Medical Director at Odessa Brown Children’s Clinic in Seattle. He describes ACEs and its impacts with KBCS’s Yuko Kodama.
Produced by Yuko Kodama and Jesse Callahan
Photo Credit: Seattle Children’s Hospital
0:00
Adverse childhood experiences or ACEs are difficult events that happened during infancy to youth. Studies have found a correlation of exposure to ACEs and long term health problems in people. Odessa Brown Medical Clinic’s medical doctor, Dr. Benjamin Danielson, speaks with KBCS’s Yuko Kodama about the study on ACEs.
0:20
The ACEs story goes back to studies done by a physician in the Kaiser Healthcare System in Southern California, who was wondering why the health outcomes for many of his adult patients were just not responding to the interventions that he was suggesting and doing. And so he started to cast this broad net and ask more and more questions. And over time found that these tenthings kept coming up in people’s backgrounds, especially large combinations of these ten things. And the most important part to me is that this was a community that was socio-economically actually relatively well off. This was community that was majority white. It was the background of these economically comfortable, mostly white, adult people who then related their stories and their experiences as children, and included these elements in them. And from that, a number of different researchers at different sites, including Harvard, and out in California, started to look at those correlations and do some of the regression analysis and the other fancy math, that then turns that into a pretty strong relationship that you can measure, count and create expectations based on.
1:37
what are some of the examples of what an adverse childhood experience could be?
1:44
The mostly things that you would recognize as unfortunate events for a child to experience, like the exposure to domestic violence in your home, the experience of having had neglect or physical punishment be a big part of your life, maybe living in a home where parents struggle with mental health conditions in a way that really adversely impacts your well being, things like that. the seriousness of adverse childhood experiences is important to think about, partly because I believe before we had much language around ACEs, many people, of course, sort of inductive knew that the hard experiences that you had, could have this impact on you, long term. But the ACEs studies actually brought that into a very, very clear light. And it’s pretty unusual, in some ways, to find something where there’s this direct correlation between the number of events and the step-wise increase in risk for illness. So I feel like it was the first time that you could pull these ideas of social exposures, things in your life happening around you, even if they’re not to you, and long term health outcomes. It’s a pretty remarkable and powerful and painful, full of a deeper story, though, than just a score, or a specific risk for heart disease, or depression.
3:13
So ACEs, does that also include things like historical trauma and epigenetics kind of things?
3:22
ACEs themselves do not include the epigenetic impacts themselves. They’re really specifically talking to the experiences that a child had, I think the continued thinking about ACEs has started to speak about community ACEs and broader generational ACEs, which does start to bring this conversation about historical trauma into scope. However, the original studies were really about what does an individual experience in their early years, how does that translate into their lifelong health? The other two important things to remember that ACEs does not speak to in any way at all. One is the impact of poverty in this country, on your health, and the other is the impact of oppression like racism on your health.
4:10
So that’s one thing, to understand it as a medical professional. And, you know, be aware of it as you’re working with people, right. But then there’s the other aspect of it, which is, medical professionals usually come into things when someone is feeling sick. So where does that put medical professionals then, in looking at this?
4:34
Such a good question. Where does that put medical professionals? Or what is where does it imply that maybe some of our training and preparation should be directed in a different way. I’m a primary care pediatrician. So I have a huge respect for prevention, and supporting wellness, not just intervening when someone is ill. Also working within those young age groups, I feel like it puts pediatricians in the space to be potentially especially impactful, on terms of affecting lifelong health. So suddenly, as a pediatrician, I feel like, I might be able to help someone who’s in their 80s down the road because of the work that you do during their childhood. The second thing for me is that as a pediatric primary care provider, among nurse practitioners, and doctors, and PAs, and all of the other wonderful types that are out there, we are all also very much involved and invested in supporting children’s social determinants, the world of exposures and experiences around them, not just their bodies, even if you think about their whole bodies, which is a stretch for some healthcare systems to think whole body, whole mind, it’s also important to be thinking whole family, whole community whole of experiences, and perhaps even the timeline of experiences, the life course, if you will, then you start to think about maybe the ACEs that mom experienced when she was a child, maybe you start to think about the genetic components that go into the creation of a child. And what ACEs those genes are exposed to. I’ve come to believe that ACEs exist within a circle of toxic stress experiences that happen in your life.
6:27
As I’ve already mentioned, the original studies were done in people with a fair amount of security economically, and who didn’t face as much racism as other people do. And so that tells me that anybody can experience a number of ACEs and they can affect your life. It also tells me that there’s a separate circle, maybe called oppression, toxic oppression, that has its own impact on your life, even if you could say that you never experienced those ten ACEs, racism and the other oppressions out there have their own impact on your well being, you can’t solve an oppression problem by saying you’re going to fix ACEs problems. But there is a huge amount of overlap and people who have to face both racism, and an ACEs score of seven, really deserve as much attention as you can provide.
7:16
And there’s a third circle, I call it toxic capitalism, other people would call it poverty. But those are all separate circles, and they can affect your well being independently or together. We’ve heard stories of Serena Williams having a near death experience in giving birth, that really almost cost her her life as a black woman in this country, not because she was socio-economically deprived, because she is in the well-to-do categories. But the racism and oppression that we have in our country have an impact on her health and her chance to have a healthy birth experience. We’ve seen plenty of folks also in low income communities who are strong together and have wonderful community experiences, and low ACEs experiences, and those communities are thriving, we should reject the idea that you have to be well off in order to thrive as a community.
8:12
So I feel that there are these three intersecting circles in our lives. And some of them overlap and some of them don’t capitalism, toxic capitalism anyway. Oppression, like racism, and marginalization, able-ism, all of those isms, the way we treat the LGBTQ community still in this country, the many different ways that we um… we other in a way that is degrading and detrimental. And then there’s a circle called toxic stress. ACEs is an important one of those. Just to make it slightly more complicated, I think there are two others in that circle too. Because I think ACEs by themselves doesn’t do justice to the stress that some people feel, you may not have had those ten things happen in your life. But you might have every single day, the trickling constant mini-crisis experiences that then wear you down that weather doesn and wear down your ability to withstand illness, to hold off emotional stress and trauma. And I think that day to day drip drop, drop of the stress hormones in your body. And those experiences in your environment also have this detrimental effect on your health. And so I don’t want to say that you only get to talk about bad health outcomes from stress if it’s in the frame of ACEs, because there are other stresses that happen.
9:36
I hear too many times a mom say ‘My car broke down last week. I had to figure out how to get alternate transportation. My job does not give me the chance to have paid leave off. And my grandmother lives far away from me now. So for me, in order for me to get to this clinic, even… to even start getting care for my child, I have to deal with all of these many crazies. And now I don’t know when I go home, whether we’re going to have food on the table that’s healthy, or whether I’m going to have to make some necessary but harder choices about the nutritional content that I’m feeding my child’ . None of those are ACEs, right? And yet, they all have a pretty important effect. And if you live through your life with those going on every day, that’s pretty hardcore.
10:18
There’s a third set that I think are mild stresses that happen at critical times in your life. And the most important example to me is childbirth. Where just something mild and unexpected happens, but it sets inside of usual sense that something else more deeply is going on, something else is wrong. I think of the mom who goes into the hospital expecting a vaginal birth, and then has a C-section occur, and everything could go great with that C-section, everything could go fine. But that is traumatic to have that change in your expectation. And I thnk there are lots of parents who then leave that experience thinking something else is wrong, something else is going to go wrong with this child because I didn’t expect that first thing to happen. And now there’s something else going on there that I think it’s not quite doing it honor to call it worried-well. There’s something in there about you’ve had an experience, not a serious, serious one. But it happened at a key time, and it changed the way you felt about how secure you are about the well-being of your child. And all of that means I think our healthcare system should be addressing those things, instead of waiting till someone’s sick and trying to treat them.
11:33
You know, medical professionals could then become advocates for the entire family, do you find yourself in that kind of position from time to time?
11:41
Yes, we’ve actually tried to structure our clinic around really thinking more environmentally more holistically about what a child needs to thrive and be happy. One example is that we’ve created a special fund that is not designated in any particular way. We call it a basic needs fund. And it’s really there to respond in the moment to the kinds of stressors that a family might experience. Just before this interview, I was weighing in on a special fund request from a family that was trying to get other family members closer to this family. They were going through a lot their child has sickle cell disease, and they really needed their whole family to kind of be together and be able to embrace, and a grandmother is living in another state. And they needed help getting that grandmother transported here. That’s so funny that ties together so many parts of what we are talking about already, but we’re able to make a contribution to the transportation needs to get grandmother into closer connection with this mom and this child, as they are managing this really hard diagnosis called sickle cell disease.
12:54
What are some of the ways that you interact with the family and your interest in the environment of a child?
13:01
I’m going to speak maybe from our best intention, best hope, best heart optimistic view. Because I don’t know if we ever get it right all the time. But I’ll share what our intentions are and how we try to make sure those are impactful.
13:17
One is that we keep trying to build more and more time into our visits, our encounters. There’s so much more to the experience and health and the well being of a child than could ever show up in a 20 minute visit, right? So we try to intentionally build a lot more time into visits, even ones that on the face of it should be brief. ‘ Can you recheck my child’s ears to make sure that ear infections getting better’. That should be you know, five minutes of peeking in an ear and talking to a mom. However, what happens so often is right near the end of that five minutes is this, oh, by the way moment, we call it, where a mom might say just’ oh, by the way, we are about to get kicked out of our apartment’ , or’ Oh, by the way, I haven’t shared this before. But we’re survivors of domestic violence. And I’m getting more worried that a threatening person is trying to, trying to find me and get back into our lives’ . And it’s , I think it’s a horrible moment in healthcare when someone would say something like, ‘ Well, good luck with that your ears are fine and see you next time’ . That would be the worst, the worst kind of care possible.
14:33
We try to make sure that we have a moment to listen, hold that space. And also, if possible, start a path of support in the, in those moments. So that takes time first. The second thing it takes is being unafraid to ask, I will share that healthcare professionals, especially young ones, come with this worry about ‘ Please don’t ask me something I don’t have an answer to’. And I get it on the one level. But it’s there’s a lot of hubris and saying I only want to have conversations when I know the answers to them. And I think that’s pretty unfortunate. Th ey’ll say stuff like I feel like It’s a harm to a family for them to share something. And for me not to be able to do something about it. And I kind of understand that. But boy, what would it be like if we all went through the world, only having conversations that we knew the end of?
15:27
Anyway, we try to build a different mentality into our clinic and say,’ Wow, that looks tough’ . And that I can only sit here and feel this with you and hold this with you. And maybe we can start to build in different kinds of responses. I mentioned our basic needs fund, which is sometimes important. We think about our care as a team. And sometimes it’s our social worker who has a connection and ability to listen in a way that is especially important and they can be part of that visit. Sometimes we need different expertise. And we have a program called a medical legal partnership, which is kind of amazing. Just what you can do, and you bring different kinds of minds together to help work on challenging problems. When it comes down to housing rights, or educational rights or access to services, the partnership between a medical person, social services person and a lawyer…that can be really powerful. So I hope that we continue to stress and push and stretch ourselves to be able to take on problems that today that feel really difficult because I think their solutions tomorrow that are going to be pretty amazing. That’s a piece of the model that we’re trying to build. We’re trying to live out where we talked about when we say that healthcare should be more integrated with lots of team members coming together in the name of supporting a child and their family and the community around them.
16:55
And then the last thing for now I’ll say is that we also try to get outside our walls as much as possible to make sure that we’re sometimes more conveniently in the spaces that feel more comfortable and safe to families in order to be good listeners in those spaces instead of on our own terms. It’s important for it not to always be a home game, right? Can I have some away games? Oh, and one other things I’ll say that structured into our visits, especially in the first year or two is we try to incorporate more of an understanding of things like parenting confidence, and the social services and support that come with that.
17:37
We try to look at more for things you would expect, like maybe postpartum mood concerns. But also we try to get a little more deeply about like, how do you feel about being a parent? How hard does it feel right now, who’s there to support you what’s important to you… em..culturally, or from a community perspective in order to, to do that as well as you want to. There are actually some evidence based screening tools that we use. One we stole from Australia. And there are some other tools that we use that are just more responsive to what the community tells us they need. We really do need to reform our healthcare training process. I feel like I experienced many, many students who came into their medical training as wonderful listeners and caring human beings full of compassion. And then the listening skill gets squeezed out. The sense of compassion sometimes gets blurred and blunted. And you see people requiring almost a period of recovery from their training in order to regain their souls. I’ll say it that way. And I think that’s just a shame.
18:49
On top of that, we create a health care system that is American, and it’s worst ways the sort of solo cowboy who’s trained to be this hero who’s going to swing into town, fix those poor deplorable people and make them better. There’s so many bad messages and the way we verbalize and don’t verbalize what we’re saying to people who go into training and healthcare. Healthcare is at its best, such a team sport, and it’s so much better actually when it’s people from many different circles. You know, take that lawyer, take that teacher, take the social worker who’s skilled in those ways, take the mental health provider, take the… maybe the health care provider hasn’t been exposed to medical school quite so much. Put them together. You’re gonna have a much better clinic or whatever you want to call it. Then you had before uncommon partnerships are so important.
19:40
That was Dr. Benjamin Danielson speaking with KBCS’s Yuko Kodama.
Transcribed by https://otter.ai
Childhood Cancer
Each year in the United States, well over 15,000 children from birth to 19 are diagnosed with cancer. KBCS’s Kendra Hanna speaks with Kelly Forebaugh of St Baldrick’s Foundation and a mother of a cancer survivor, about how treating cancer in children is different than cancer treatment for adults.